Diet and Health: With key to the calories. Lulu Hunt Peters, 1918
By Sally J. Feltner, PhD, RDN
In 2013, the American Medical Association House of Delegates approved a resolution classifying obesity as “a disease state with multiple pathophysiological aspects requiring a range of interventions.” We now accept the fact that obesity can lead to diabetes, heart disease, and cancer risks.
Today, 2.1 billion people – nearly 30% of the world’s population – are either obese or overweight, according to new data from 188 countries. The U.S. Centers for Disease Control and Prevention analysis said, “About 38 percent of U.S. adults aged 20 and older are obese as are more than 17 percent of children aged 6 to 11, federal data shows.”
“The global problem affects all countries, income levels, age groups and accounts for over 3-4 million deaths a year with estimated health costs of over $2 trillion a year.” (International Journal of Obesity).
There is no one cause. Many people still continue to blame the obese person’s lack of willpower and insist that if they just ate less and moved more, their weight would not be a problem. This may explain some cases of obesity, but how could more than 2 billion people worldwide begin to make poor choices about their food intake and allow themselves to become fat. Moreover, this upward trend earnestly began in the late 1980’s and has continued to the present. Obesity rates were just 13.4% in 1980 but reached 34.3% by 2008. So what happened to cause this sharp rise? – More than likely a lot of things.
In 2016, an article by Bruce Y. Lee, Associate Professor of International Health at Johns Hopkins Bloomberg School of Public Health succinctly describes his opinions on what factors changed to help create this epidemic. He states that obesity is a result of the breakdown of three major systems that include biological, social, and environmental factors.
Biological Systems
Our metabolic systems have been affected to some extent by non-stop dieting. A plethora of fad diets and exercise gimmicks grew into a huge obesity industry. Diet books topped Amazon and best seller lists while the supplement industry went berserk over worthless and sometimes dangerous weight loss aids. Americans responded and when surveyed, a large majority of respondents said they were “on a diet.”
Even TV reality shows (The Biggest Loser) resulted in weight loss that lowered the metabolism of almost all participants gained back their hard-fought loss. As each weight loss attempt occurs, the cycle of weight loss/regain occurs over and over again. The body is threatened by a perceived starvation state and attempts to prevent it by putting forth metabolic and hormonal mechanisms to alleviate the threat. Obesity research has shown that nearly 95% of dieters regain their weight loss in a few years.
Social Systems
Social media, friends and family, cultural beliefs, TV advertising, and personal responsibility are all important in shaping our behaviors about eating, appearance, and body image.
Advertisements in the media have promoted the obesity epidemic by making claims that their products will magically transform your body into a svelte image and allow you to finally wear that bikini you bought years ago and that weight loss is easy. Most weight loss diets promise success by showing us before and after pictures of supposedly successful weight losers. What they do not say but disclaim in the small print that you usually can’t read is that results don’t always occur as presented. Most weight loss programs do not include an exercise component nor do they offer any behavioral counseling. Almost all have no disclosure about their success rates of weight loss and maintenance.
Environmental Systems
Determining what a healthy diet consists of is difficult enough – opinions abound and debates continue. This results in confusion and misinformation for the average consumer. They tend to give up on just what exactly is the best way to eat.
So many individuals are exposed to reliance on cheap foods found in the fast food industry. They may live in food deserts defined as parts of the country usually found in impoverished areas devoid of easy access to fresh fruit, vegetables, and other healthful whole foods. This is largely due to a lack of grocery stores, farmers’ markets, and other healthy food choices.
The food industry has been instrumental in developing ultra-processed foods that hardly resemble “real” foods. Snacking has become a national pastime and is dominating several of the inner aisles of the supermarkets. Snacks are abundant in every gas station, convenient store, or vending machine that tempt you to increase their profits.
Additionally, the food industry promotes the intake of sugar, fat and salt by attempting to reach what they call “the bliss point,” defined by the precise amount of sweetness that makes food and drink most enjoyable. You can find the results in the sugary cereals and sweetened beverage aisles in the supermarkets.
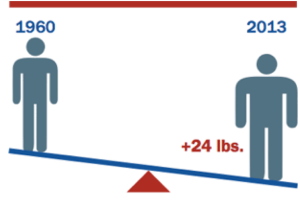
People do not cook anymore leading to procuring your meals outside the home. Restaurant portions have become gigantic compared to what they were in past decades. For example, a typical serving of theater popcorn was 270 calories (5 cups) in 1970 compared to now that is typically 630 calories (one tub). Some restaurant meals contain as many calories as we need in an entire day. The average U.S. intake increased 455 kcal/day, a 20% increase from 1970 to 2009. (Dr. Stephen Guyenet, The American Diet, 2012). From research studies we have found that the more food that is put in front of people, the more they eat. We now are familiar with the term “supersize” and the concept of “all you can eat buffets.”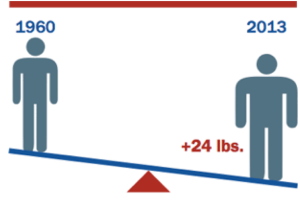
The complexities of the obesity epidemic/pandemic are impossible to fully comprehend as well as their need to be “fixed” to reverse or at least slow down the trend. There are some solutions to accomplish this but they will require much cooperation between politics, community, medicine, research, government, and the public.
If America’s obesity trend continues at its current pace, all 50 states could have obesity rates above 44 percent by 2030, according to a new report from Trust for America’s Health and the Robert Wood Johnson Foundation. Although important, we need to stop just focusing on what we eat, but equally important on how we eat to fix what contributed to the epidemic in the first place.



 Experts suggest that more than 5.5 million Americans may have Alzheimer’s disease (AD), the most common cause of dementia, i.e., Alzheimer’s’ disease may affect about 1 in 9 people. Dementia is the loss of cognitive functioning that can interfere with a person’s daily life and activities. AD is currently ranked as the sixth leading cause of death in the U.S.
The causes of dementia can vary depending on the type that also includes not only AD, but Lewy body dementia or vascular dementia and it is common for people to have a combination of two types.
AD is named after Dr. Alois Alzheimer in 1906 after he noted symptoms of memory loss, language problems and unpredictable behaviors in a female mental illness patient. After her death and autopsy of her brain, he reported he found abnormal clumps that are now referred to as amyloid plaques and tangled bundles of fibers now called neurofibrillary or tau tangles. It is thought that these abnormalities stop the function of healthy neurons that ultimately lose their connections and die.
The causes of AD are unknown, but can be combinations of genetics, environmental and lifestyle factors. An improper diet has been suggested as a possible contributor by inflicting free radical or inflammatory damages. Positive dietary adjustments may also play a role in preventing the disease. Recently animal research has investigated other prevention treatments that may help to allay the effects of lifestyle factors on Alzheimer’s disease.
“The
Experts suggest that more than 5.5 million Americans may have Alzheimer’s disease (AD), the most common cause of dementia, i.e., Alzheimer’s’ disease may affect about 1 in 9 people. Dementia is the loss of cognitive functioning that can interfere with a person’s daily life and activities. AD is currently ranked as the sixth leading cause of death in the U.S.
The causes of dementia can vary depending on the type that also includes not only AD, but Lewy body dementia or vascular dementia and it is common for people to have a combination of two types.
AD is named after Dr. Alois Alzheimer in 1906 after he noted symptoms of memory loss, language problems and unpredictable behaviors in a female mental illness patient. After her death and autopsy of her brain, he reported he found abnormal clumps that are now referred to as amyloid plaques and tangled bundles of fibers now called neurofibrillary or tau tangles. It is thought that these abnormalities stop the function of healthy neurons that ultimately lose their connections and die.
The causes of AD are unknown, but can be combinations of genetics, environmental and lifestyle factors. An improper diet has been suggested as a possible contributor by inflicting free radical or inflammatory damages. Positive dietary adjustments may also play a role in preventing the disease. Recently animal research has investigated other prevention treatments that may help to allay the effects of lifestyle factors on Alzheimer’s disease.
“The 
 The most talked about topic concerning our obesity epidemic involves two major theoretical theories: the conventional theory of calories in -calories- out and the carbohydrate-insulin model. It is important for the population to have a basic understanding of these theories in order to deal with the obesity conundrum so prevalent in our current food environment. Determining which is predominant could help us to counteract the epidemic with the most effective dietary treatments. The following article provides us with a simplified understanding of both sides of the debate.
The most talked about topic concerning our obesity epidemic involves two major theoretical theories: the conventional theory of calories in -calories- out and the carbohydrate-insulin model. It is important for the population to have a basic understanding of these theories in order to deal with the obesity conundrum so prevalent in our current food environment. Determining which is predominant could help us to counteract the epidemic with the most effective dietary treatments. The following article provides us with a simplified understanding of both sides of the debate.